The Best TSH-Producing Pituitary Adenoma Treatment in Guntur
Continuous stimulation of the thyroid gland by excessive pituitary secretion of TSH may cause a hyperactive thyroid gland (hyperthyroidism). A TSH-producing pituitary adenoma makes too much thyroid-stimulating hormone, which stimulates the production of thyroid hormones from the thyroid gland. These hormones regulate metabolism and affect other organs’ growth and rate of function. Dr. Rao’s hospital is the best neurosurgery hospital with the best neurosurgeon Dr. Mohana Rao Patibandla being the best neurosurgeon in India.
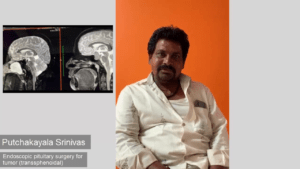
The best transnasal transsphenoidal surgery – complete removal of pituitary tumor
About TSH-Producing Adenomas
A TSH-producing pituitary adenoma is the least common type of pituitary adenoma, occurring in only 1% to 3% of all pituitary adenomas. This type of tumor is more common in females. The tumors are often greater than 1 cm in diameter, referred to as a macroadenoma. It needs a multidisciplinary team to treat the tumor together, including an endocrinologist, a neurosurgeon, an ophthalmologist, and a radiologist.
With successful multidisciplinary treatment, hormone levels can return to normal, and the tumor can be removed.
Symptoms
Symptoms of hyperthyroidism include:
- Nervousness
- A fast heartbeat
- Weight loss
- Frequent bowel movements
- Difficulty sleeping
- Tremor of the hands
- Less menstrual flow
- loss of menstrual periods
- Fatigue
Other symptoms of pituitary tumors are:
- Visual loss
- Headache
Diagnosing TSH-Producing Adenomas
There are no known steps to prevent TSH-producing adenomas, but early diagnosis improves the chance of cure with surgery alone.
A diagnosis is confirmed by:
- Blood tests: In general, elevated T3 and T4 in normal or high TSH presence suggests a TSH-producing tumor. In some cases, thyroid hormones are normal despite the presence of a tumor. This is called a silent TSH adenoma.
- MRI or CT scans: The presence of a pituitary adenoma in the MRI study usually shows a large tumor; however, some tumors may be too small to see.
Treatment
Early treatment prevents the progression of visual loss and headaches caused by many larger tumors.
The goals of treatment are to:
- Restore production of TSH and thyroid hormones to normal
- Stop and reverse the symptoms of TSH-producing adenomas
- Correct other endocrine abnormalities (adrenal, ovaries, or testes)
- Remove and destroy the tumor to restore endocrine function to standard and to relieve any symptoms directly related to the tumor
Medical Therapy
Medical treatment for this type of tumor is a somatostatin analog. This drug acts on the tumor to lower TSH production, which results in lowering both TSH and thyroid hormone levels.
Some patients have a decrease in tumor size as well. Some patients have been treated successfully only with an injection in the buttock once a month and have not required surgery. This drug does not destroy the tumor; it’s only effective as long as it is administered, so it’s not a cure.
Surgery
Surgery is the most common treatment for TSH-producing adenomas and uses a transsphenoidal approach. The operation is performed through the nose without disturbing the brain or the eye nerves. To protect against heart problems during surgery, TSH-producing tumors require treatment early. This treatment usually takes 3-4 weeks and includes a beta-blocker to slow the heart rate and a drug that reduces the amount of thyroid hormone production.
After Successful Surgery
Once the tumor is completely removed, normal thyroid hormone production resumes. Although hormone levels will return to normal within days, the symptoms of a TSH-producing adenoma may take days to weeks to resolve.
Some patients may have deficient TSH levels after surgery. These patients may need thyroid hormone replacement either temporarily or permanently.
Radiation Therapy
Radiation therapy or radiosurgery are options for patients with persistent elevation of TSH despite medical therapy or patients who can’t receive medical therapy for one reason or another. Conventional radiation therapy is effective but involves a 4-6 week treatment period.
A single treatment with Stereotactic Radiosurgery has been a successful option and has the potential to provide excellent long-term control.
After Treatment
Your pituitary tumor may recur at any time, so you’ll need regular follow-up visits with blood tests and possibly an MRI scan. You’ll need additional treatment if your tumor recurs.
