Why Choose Dr. Rao’s Hospital – the best neurology hospital?
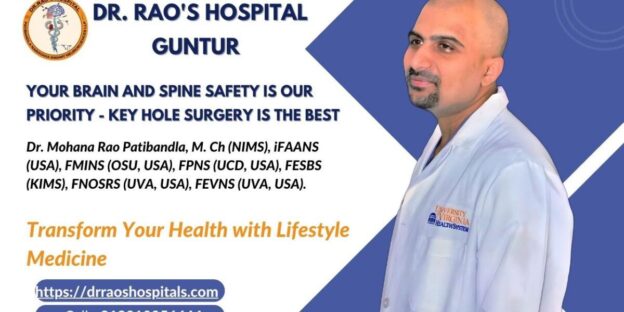
Welcome to Dr. Rao’s Hospital, your trusted destination for Comprehensive Neurology Care in Guntur!
Are you searching for the best neurology hospital in Guntur? Look no further! At Dr. Rao’s Hospital, we pride ourselves on being a beacon of excellence in the field of neurology. Our dedicated team of neurologist specialists in Guntur is committed to providing you with unparalleled medical care and expertise.
Why Choose Dr. Rao’s Hospital?
Best Neurologist Doctors in Guntur:
Our hospital boasts a team of the top neurologist doctors in Guntur who are renowned for their expertise and compassionate patient care. With a focus on accurate diagnosis and personalized treatment plans, our neurologists are dedicated to improving your neurological health.
Top Neurologist in Guntur:
Dr. Rao’s Hospital stands out as the home of the top neurologist in Guntur. Our specialists possess extensive experience and are equipped to address a wide spectrum of neurological conditions, from common ailments to complex disorders.
Neuro Physician in Guntur
Looking for a skilled neuro physician in Guntur? Your search ends here. Our neurologists combine advanced medical knowledge with a patient-centric approach, ensuring you receive the best possible care for your neurological concerns.
Brain Specialist in Guntur:
Dr. Rao’s Hospital takes pride in being a trusted brain specialist in Guntur. Our expertise covers a range of neurological disorders, with an emphasis on accurate diagnosis and holistic treatment plans.
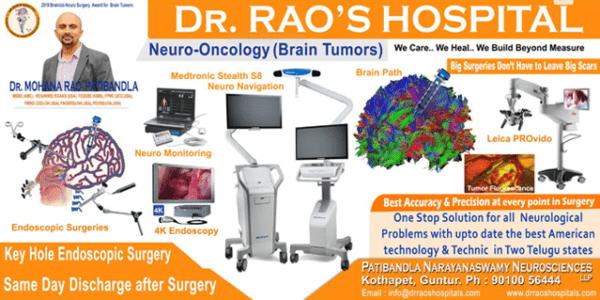
Best Neurosurgeon in South India
Are you in need of a neurosurgeon? Our hospital is proud to have the best neurosurgeon in South India, renowned for their surgical excellence and dedication to patient well-being.
Spine Specialist Hospital:
Searching for the best spine care hospital in Guntur? Look no further. Dr. Rao’s Hospital offers cutting-edge spine care services, backed by a team of skilled professionals who specialize in neurosurgical spine procedures.
Paediatric Neurologist Near Me:
Our hospital understands the unique needs of pediatric patients. With a paediatric neurologist near you, we provide specialized care to ensure the well-being of your child’s neurological health.
Neurosurgeon Spine Surgeon:
Our team includes a dedicated neurosurgeon spine surgeon who specializes in intricate spine surgeries. Whether it’s spinal deformities or complex injuries, our experts are equipped to provide exceptional care.
Best Hospital for Back Problems:
If you’re seeking the best hospital for back problems, your search concludes at Dr. Rao’s Hospital. Our multidisciplinary approach ensures comprehensive care for all types of back issues. According to mid-day
Neuro Spinal Hospital Location:
Located conveniently, Dr. Rao’s Hospital serves as a leading neuro spinal hospital. Our strategic location ensures easy accessibility for patients seeking specialized neurological and spinal care.
Neurology Appointment Near Me:
Need a neurology appointment near you? Our hospital offers timely appointments with our experienced neurologists, ensuring you receive the attention you deserve.
Brain Tumor Best Treatment in India:
If you’re seeking the best brain tumor treatment in India, you’re in capable hands at Dr. Rao’s Hospital. Our expertise in brain tumor care ensures optimal treatment outcomes.
At Dr. Rao’s Hospital, we are committed to transforming lives through comprehensive neurology care. Our state-of-the-art facility, coupled with the expertise of the best neurologist and neurosurgeon in Guntur, ensures that you receive world-class treatment for your neurological needs.
Ready to take charge of your neurological health? Contact us today to schedule your appointment and experience the difference that expertise and compassion can make in your journey towards a healthier life.
Visit our website for more information drraoshospitals or call us at 9010056444. Your neurological well-being is our top priority!